Vocal Fold Paralysis
Regain Your Voice After Vocal Fold Paralysis. Specialized voice therapy to restore clear, strong voicing—even in complex cases of unilateral or bilateral paralysis.
Voice Therapy for Vocal Fold Paralysis
Voice rehabilitation after unilateral or bilateral vocal fold paralysis is a real challenge with which I have specialized over the past 25 years.
The first and foremost is for each patient to understand that there are options for voice recovery! You are not stuck with a terminal diagnosis!!!!
Waiting for time to pass is just one of your options and, in my experience, not often the ideal option!!!
Unilateral Vocal Fold Paralysis
Voice Therapy intervention with the IVT approach aims for total voice rehabilitation.
- Success rates are very high. At an average of 8-12 therapy sessions there is a recovery rate for 80-90% of cases with unilateral vocal fold paralysis and voice returns to comfortable and lour voicing with a comfortable and natural breathing pattern.
- Even for the cases where for various reasons, organic and/or psychoemotional, we can not achieve a complete voice rehabilitation, there is a notable improvement with both ease of voicing as well as a more comfortable breathing coordination so that the patient no longer feels out of breath.
- Referrals to other relevant specialists is frequently necessary due to the multilayered difficulties related to vocal fold paralysis. Voice physiotherapy has been the specialization which I have found most valuable for assisting the efficacy of the voice therapy techniques.
- Not all cases are success stories and there are cases when re-evaluation of our progress may lead us in a different direction.
Bilateral Bocal Fold Paralysis
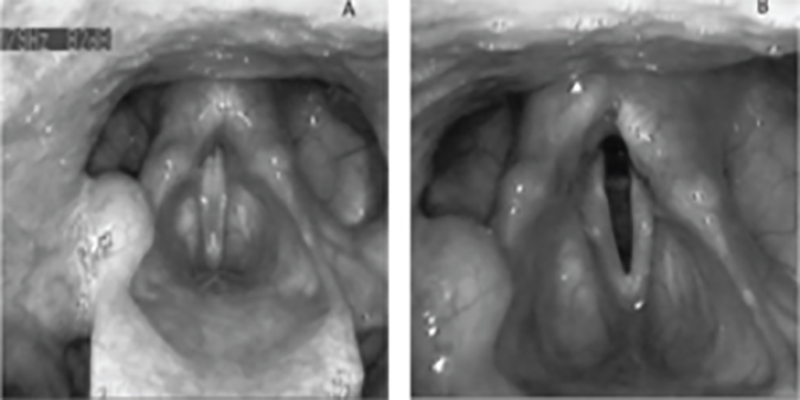
Voice and breathing rehabilitation for cases of bilateral vocal fold paralysis is a great challenge for both the patient and the therapist. For patients, the prevalent distressing symptoms involve the feeling of an inadequate breath supply while, depending on the position of the paralyzed vocal folds, quality of voice is also impaired to a greater or lesser degree.
To my knowledge, there is no evidence based research to guide clinical voice therapy techniques for rehabilitating this particular group of patients. However, as the numbers of cases that came to my clinic with these complaints started increasing over the past decade, my team and I decided we needed to come up with some sort of strategy to help out. Over the years, we persevered and have arrived at a strategy that has offered impressive results for a significant proportion of our patients. This clinical based evidence is what we have to offer, for now, to the scientific community.
Let’s take it from the top and once again acknowledge the importance of the 18-24 month waiting period before the ENT can definitively diagnose a permanent paralysis. If the neurological trauma is permanent, depending on the degree of breathing and voicing difficulties, the ENT Surgeon and the multidisciplinary team can assist the patient with consideration of the options for improvement of breathing and voicing.
Technological advances are moving closer towards being able to offer permanent solutions. Laryngeal pacemakers are developing and have offered impressive results in certain cases.
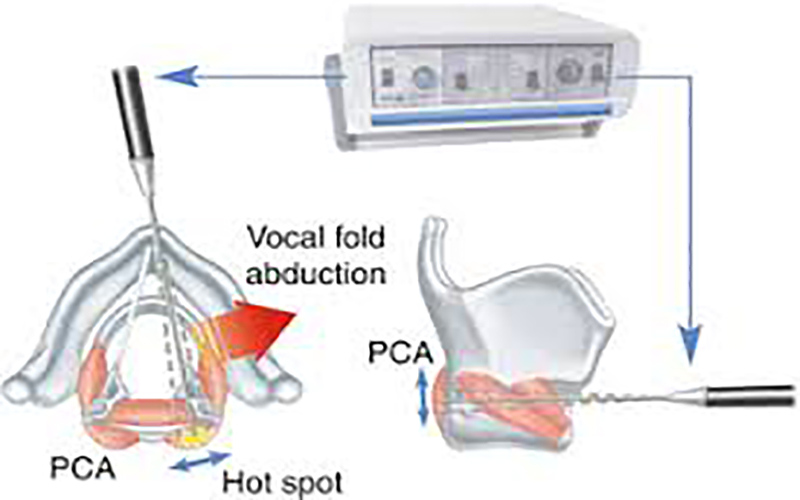
The Aim of the Laryngeal Pacemaker
In simplified terms, the aim is to direct an electrical impulse to the vocal fold(s) so that it is drawn open for inspiration and closes for expiration and speech, resulting in manageable breath and voice. I believe there are specific prerequisites for a patient to be considered for a laryngeal pacemaker.
There are also various surgical options for achieving improved airway patency. However, depending on particular surgical details there is a significant chance that, although airway patency can successfully be achieved, in certain cases the voice deteriorates significantly. Happily, there are also numerous cases where surgical intervention improves airway patency while also maintaining excellent voicing. Is is my understanding that the success of the surgical intervention depends on a number of critical factors including the experience and skill of the ENT surgeon, the strategy and surgical technique that will be used as well as patient-specific prerequisites. For patients considering surgical intervention, I would recommend discussing all the relevant details with your ENT surgeon so that you are well informed of all the pros and cons of the procedure and in a position to make an informed decision.

